
Breast Screening Mammograms
“The biggest catastrophe in women’s health is taking place right before our eyes. Healthy women all over the world have been disfigured and brainwashed into believing that their beautiful nurturing breasts have only one objective… to kill them.“
The promise (film)
What are mammograms?
A mammogram is an X-ray picture of the breast. Doctors use a mammogram to look for early signs of breast cancer when there are no symptoms. Mammograms may also be used to detect breast cancer in men if there is enough breast tissue.
Do Screening Mammograms save lives?
In this study 89,835 women aged 40-59 were randomly assigned to mammography (five annual mammography screens) or control (no mammography). The study found that annual mammograms did not reduce death from breast cancer…
A Cochrane review of 10 trials involving more than 600,000 women showed no evidence that mammography screening reduced overall mortality (deaths).
In 2013, the Swiss Medical Board recommended that Mammography Screening be abolished in Switzerland ( The New England Journal of Medicine ) because of the emerging evidence that the harms of mammography outweigh the benefits.
The following is worth noting:
In his editorial on the study, Chief Medical Officer for the American Cancer Society, Dr. Otis Brawley recognises the need for accepting the limitations of mammography screening, “Acknowledging the existence of breast cancer overdiagnosis challenges the value of screening: it means that the benefits of breast screening have been overstated, and that some women who have been “cured” were harmed because they received unnecessary treatment”.
The main findings from the study are that:
- Screening did not reduce the number of late stage tumours (those bigger than 2 cm), which means that breast screening is unlikely to reduce breast cancer mortality or lead to less invasive treatment
- 1 in 3 breast cancers detected in women offered screening are likely overdiagnosed
Should mammography screening be stopped?
Independent expert groups in Switzerland and France have recommended that breast screening be stopped or reduced substantially. Elsewhere, guidelines are already changing as well, i.e. the American Cancer Society now recommend less frequent screening of a narrower age group than just two years ago. Our study supports this development.
The full report is titled: “Breast Cancer Screening in Denmark: A Cohort Study of Tumor Size and Overdiagnosis.” The authors are K.J. Jørgensen, P.C. Gøtzsche, M. Kalager, and P. Zahl.
Abolishing Mammography Screening Programs? A View from the Swiss Medical Board (published in The New England Journal of Medicine) was written by Nikola Biller-Andorno, M.D., Ph.D., and Peter Jüni, M.D. – two members of the expert panel mandated to prepare a review of mammography screening in Switzerland. In the article they say:
It is easy to promote mammography screening if the majority of women believe that it prevents or reduces the risk of getting breast cancer and saves many lives through early detection of aggressive tumors.
We would be in favor of mammography screening if these beliefs were valid. Unfortunately, they are not, and we believe that women need to be told so. From an ethical perspective, a public health program that does not clearly produce more benefits than harms is hard to justify. Providing clear, unbiased information, promoting appropriate care, and preventing overdiagnosis and overtreatment would be a better choice.
No Mortality Benefit of Breast Cancer Mammography Screening in 25-Year Follow-up of Canadian National Breast Screening Study
By Matthew Stenger The ASCO Post
As reported in BMJ by Anthony B. Miller, MD, Professor Emeritus at the Dalla Lana School of Public Health, University of Toronto, and colleagues, the 25-year follow-up of the Canadian National Breast Screening Study has shown no mortality benefit of annual mammography screening for breast cancer compared with physical examination or usual care. Mammography screening was associated with substantial overdiagnosis…
…By the end of the 5-year screening period, there were 142 excess cases of breast cancer in the mammography group (666 vs 524). At 15 years after enrollment, the excess number of cancers in the mammography group became constant at 106 cancers. The excess number represents 22% (106/484) of all screen-detected cancers. Thus, there was one case of overdiagnosis of breast cancer for every 424 women screened by mammography during the trial.
The investigators concluded, “[O]ur data show that annual mammography does not result in a reduction in breast cancer specific mortality for women aged 40 to 59 beyond that of physical examination alone or usual care in the community. The data suggest that the value of mammography screening should be reassessed.”
Continue reading at The ASCO Post
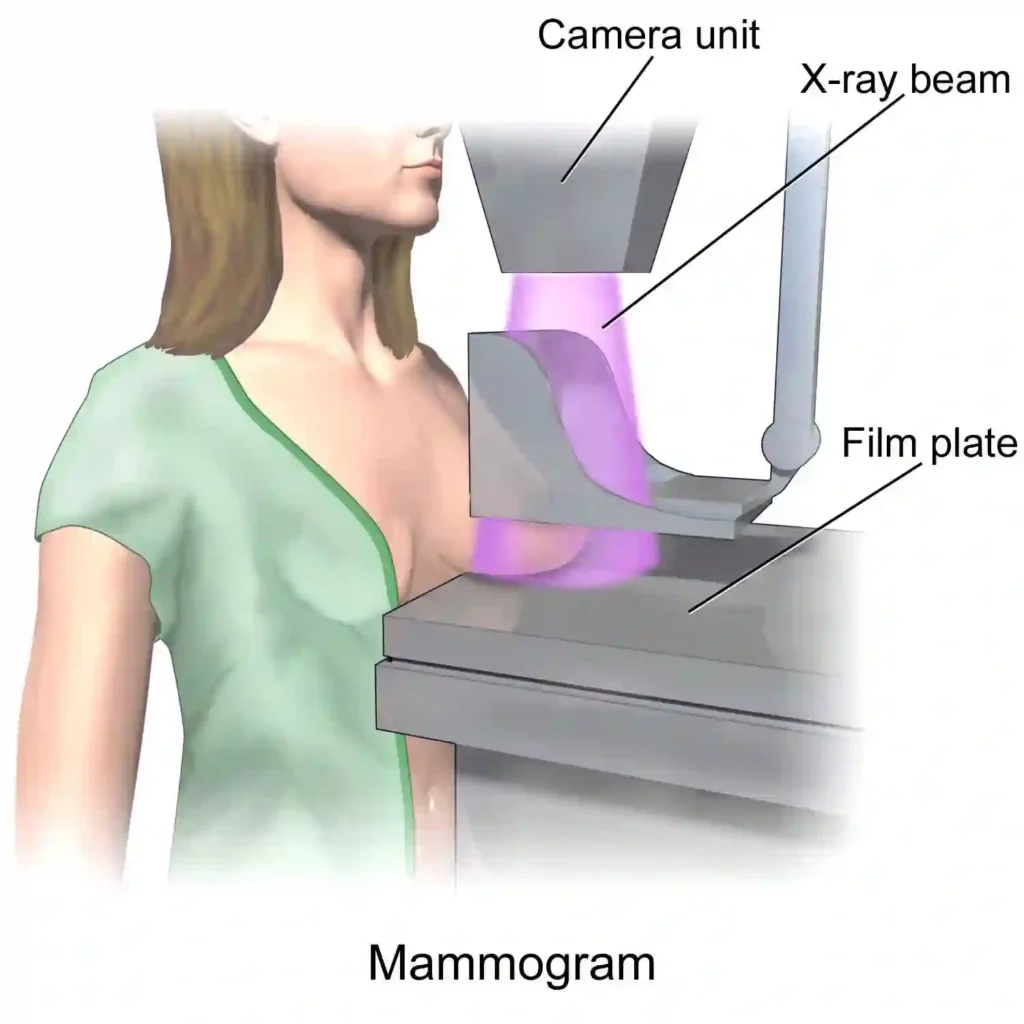
Pic credit: Title: Mammogram Author: Blausen.com staff
Source: Wikipedia License: Creative Commons Attribution 3.0 Unported.
Mammography’s big failing: Overdiagnosis
Definition of Overdiagnosis
Source: National Cancer Institute
Finding cases of cancer with a screening test (such as a mammogram or PSA test) that will never cause any symptoms. These cancers may just stop growing or go away on their own. Some of the harms caused by overdiagnosis are anxiety and having treatments that are not needed.
Some cancers that are diagnosed early do not develop symptoms requiring treatment, while others grow so slowly that the patient outlives the cancer and dies of other causes. Many of these are treated unnecessarily, leading to:
- Unnecessary tests and treatment
- Exposure to dangerous side-effects
- Radiation-induced cancers
- Mental and physical pain
- Infertility
- Inflated survival rates
This study says: We have also confirmed…our earlier finding that screening leads to more aggressive treatment, increasing the number of mastectomies by about 20% and the number of mastectomies and tumourectomies by about 30%…Furthermore, carcinoma in situ does not always develop into invasive cancer, but since these early lesions are often diffuse, women are sometimes treated by bilateral mastectomy. Therefore, the increase in surgery rates could also be an underestimate, since reoperations and operations in the contralateral breast seemed not to have been included.
New study finds breast cancer screening leads to substantial overdiagnosis
News Release issued by Nordic Cochrane Center
Women have been told for decades that they need to attend their routine breast screening appointments to detect early signs of breast cancer. However, a new major study, conducted by researchers at the Nordic Cochrane Centre in collaboration with researchers from Norway, looked into the effects of breast cancer screening programmes and have found a high risk of overdiagnosis and raise doubt about their benefits.
Risk of overdiagnosis outweighs the advantages of breast screening programmes. The cohort study, which was recently published in Annals of Internal Medicine, supports previous findings from the Cochrane review: Screening for breast cancer with mammography on the high risk of overtreating women and the doubts raised about the benefit of the intervention.
In an attempt to diagnose breast cancer early, a mammography screening very often detects small tumours that might not necessarily become malignant. In other words, the tumour would more than likely not be a life-threatening illness or health problem for the woman being treated. A breast cancer diagnosis is a life-changing event with profound implications for the psychological well-being and quality of life for women diagnosed and their families. They are subjected to invasive surgery, radiotherapy and sometimes chemotherapy, all of which are known to have serious, sometimes lethal, harms. The study also found that screening did not reduce the number of late stage tumours (those bigger than 2 cm), which means that breast screening is unlikely to reduce breast cancer mortality or lead to less invasive treatment.
Karsten Juhl Jørgensen, the lead author of the study explains, “In Denmark, we have the conditions to carry out a unique study as the screening programme was rolled out across the country in different regions at different times. We, therefore, had a control group of women of the same age during the same time period where the screening programme existed. This group of women were not screened over a 17-year period, making it possible for us not to have to speculate over what would have happened in the absence of screening”.
Additionally, breast screening leads to a 25 % to 50 % risk of being recalled due to a false positive test result if women attend a screening for the often recommended 20-year period. A false positive recall often means more mammograms and often biopsies. The time until a breast cancer diagnosis is excluded can be very stressful, and can have negative implications for many women’s quality of life even well beyond this period.
This study of all women aged above 30 years (4.3 million, in 2000) in Norway and Sweden, says:… We conclude that after the introduction of screening programmes in Norway and Sweden one third of all cases of invasive breast cancer in the age group 50-69 are overdiagnosed—that is, without screening these cases would not have been detected during the patients’ lifetime.
A study published in 2017 in the New England Journal of Medicine involving thousands of breast cancer cases, concluded that a significant proportion of tumors detected through mammography are not small because they are found early. Instead, the tumors are small because they are biologically prone to slow growth.
The National Cancer Institute Breast Cancer Screening (PDQ®) Health Professional Version (2018) includes the following admission: A population-based study in the Netherlands showed that about one-half of all screen-detected breast cancers, including DCIS, would represent overdiagnosis and is consistent with other studies, which showed substantial rates of overdiagnosis associated with screening.
In an interview with National Public Radio, Donald Lannin, a professor of surgery at the Yale School of Medicine, who led the study, said “It takes 15 or 20 years for [these small tumors] to cause any problems. And you can kind of imagine that a lot of patients will die of something else over that 15 or 20 years.
That means a significant proportion of women who get screened for breast cancer with a mammogram go through biopsies, surgery, chemotherapy, radiation and experience a lot of stress for tumors that may never pose a health threat.
In the same interview, H. Gilbert Welch, a professor of medicine, community and family medicine at Dartmouth College, who was not involved in the study, said “It appears that screening disproportionately finds good cancers” cancers that may be better off not found,”
“I think that we all need to realize that we’ve probably oversold the idea that looking for cancer early is the best way to avoid it,” Welch says. “Mammography’s a really close call. It’s a choice. We’ve exaggerated its benefit and we’ve sort of understated its harms.”
More studies
A study published in 2017 in the New England Journal of Medicine involving thousands of breast cancer cases concluded that a significant proportion of tumors detected through mammography are not small because they are found early. Instead, the tumors are small because they are biologically prone to slow growth.
This study found mammograms can result in over diagnosis and unnecessary treatment.
This study involving 50-year-old Finnish women attending their first breast cancer screening found that mammograms can also be very painful. Sixty-one per cent reported painful and 59% uncomfortable mammograms (4% severely).
The authors of this study which looked at cancer overdiagnosis stated: We estimate the magnitude of overdiagnosis from randomized trials: about 25% of mammographically detected breast cancers…
This Article, published in 2012 in the New England Journal of Medicine, found: 31% of all breast cancers are over-diagnosed.
This 2016 review concluded:
· At least 20% of Breast Cancer patients, if left untreated would be alive after 5 years
· limited evidence suggests that around 10% of screen detected Breast Cancers may regress.
This study says:
Invasive breast cancer
Of screening-detected invasive breast cancers, up to 30% might be ultra-low risk on the basis of their molecular profile. … Molecular classifiers are used to avoid chemotherapy, but could also classify tumours that have a very low or no risk of metastatic progression after simple excision, supporting the safe elimination of radiation therapy after lumpectomy in postmenopausal women, benefiting many women.
The National Cancer Institute’s Breast Cancer Screening (PDQ®)–Health Professional Version (updated June 1, 2018) includes the following :
Theoretically, in a given population, the detection of more breast cancers at an early stage would result in a subsequent reduction in the incidence of advanced-stage cancers. This has not occurred in any of the populations studied to date. Thus, the detection of more early stage cancers likely represents overdiagnosis. A population-based study in the Netherlands showed that about one-half of all screen-detected breast cancers, including DCIS, would represent overdiagnosis and is consistent with other studies, which showed substantial rates of overdiagnosis associated with screening.
Ductal carcinoma in situ
Ductal carcinoma in situ is a pathological entity that is an unintended result of breast cancer screening, rarely diagnosed before screening was adopted. Diagnosis of ductal carcinoma in situ results in immediate treatment with aggressive locoregional therapy; however, the natural history of untreated ductal carcinoma in situ has never been elucidated. Results of studies suggest that only a subset of ductal carcinoma in situ progresses to clinically significant invasive cancer during a patient’s lifetime. The result of this historically aggressive treatment approach is that nearly 50 000 women per year in the USA are diagnosed and given treatment, 20 000 of whom undergo mastectomy, with a growing proportion opting for bilateral mastectomy.
[These women believe screening and treatment saved their lives when in fact they did not need any treatment at all.]
The view of some health professionals
In an interview with National Public Radio, Donald Lannin, a professor of surgery at the Yale School of Medicine, who led the study, said “It takes 15 or 20 years for [these small tumors] to cause any problems. And you can kind of imagine that a lot of patients will die of something else over that 15 or 20 years.
That means a significant proportion of women who get screened for breast cancer with a mammogram go through biopsies, surgery, chemotherapy, radiation — and experience a lot of stress — for tumors that may never pose a health threat.”
In the same interview, H. Gilbert Welch, a professor of medicine, community and family medicine at Dartmouth College, who was not involved in the study, said “It appears that screening disproportionately finds good cancers — cancers that may be better off not found,”. “I think that we all need to realize that we’ve probably oversold the idea that looking for cancer early is the best way to avoid it,” Welch says. “Mammography’s a really close call. It’s a choice. We’ve exaggerated its benefit and we’ve sort of understated its harms.”
Some Solutions
1. MRI and mammography
This study concluded:
Screening with both MRI and mammography might rule out cancerous lesions better than mammography alone in women who are known or likely to have an inherited predisposition to breast cancer.
2. Reclassification of some “cancers”
Renaming low risk conditions labelled as cancer
Source: BMJ
Removing the cancer label in low risk conditions that are unlikely to cause harm if left untreated may help reduce overdiagnosis and overtreatment…Evidence is mounting that disease labels affect people’s psychological responses and their decisions about management options. The use of more medicalised labels can increase both concern about illness and desire for more invasive treatment.
This study says: A vast range of disorders—from indolent to fast-growing lesions—are labelled as cancer. Therefore, we believe that several changes should be made to the approach to cancer screening and care, such as use of new terminology for indolent and precancerous disorders. We propose the term indolent lesion of epithelial origin, or IDLE, for those lesions (currently labelled as cancers) and their precursors that are unlikely to cause harm if they are left untreated.
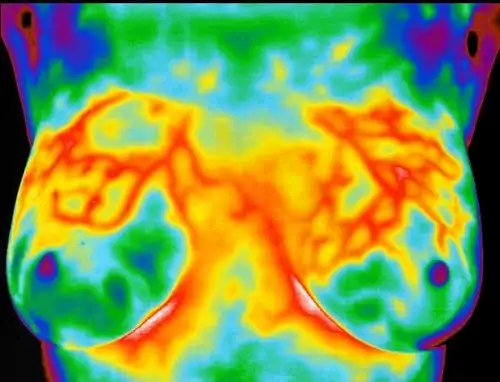
3. Alternative Screening Method: Digital Infrared Imaging (Thermography)
Alternative Screening Method: Thermography
Digital Infrared Imaging as a risk marker for breast cancer
Source: breastthermography.com
Studies show that an abnormal infrared image is the single most important marker of high risk for developing breast cancer, 10 times more significant than a family history of the disease (5). Consequently, in patients with a persistent abnormal thermogram, the examination results become a marker of higher future cancer risk (4,5). Depending upon certain factors, re-examinations are performed at appropriate intervals to monitor the breasts. This gives a woman time to take a pro-active approach by working with her doctor to improve her breast health. By maintaining close monitoring of her breast health with infrared imaging, self breast exams, clinical examinations, mammography, and other tests, a woman has a much better chance of detecting cancer at its earliest stage and preventing invasive tumor growth.
Angiogenesis, or new blood vessel formation, is necessary to sustain the growth of a tumor. Digital Infrared Imaging may be the first signal that such a possibility is developing .
See full article at breastthermography.com
Where can I get this test?
Ireland: Thermography Clinic Ireland
United States: Breast Thermography (list of testing centers country-wide)
Dr H. Gilbert Welch on the pros and cons of Mammograms
View an eye-opening documentary on breast screening at thepromisefilm.net
Should you undergo regular mammograms?
That’s your call. The above information is for educational purposes only.
If you notice any symptoms or changes in your breasts, you should consult your GP without delay.
Breast Cancer
Updated 2024

